News
Researching the Future of Cancer Treatment
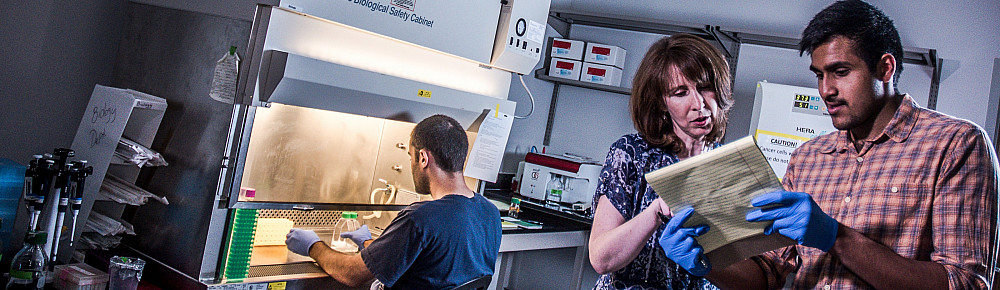
Professor of Biology Maria Todd mentors undergraduates while examining the mechanics of how cancer spreads.
November 07, 2019
November 07, 2019
Maria Todd would probably prefer that I write this story about … well, anyone else but her. When I first interviewed her and began with the warm-up question of how long she’s been researching and teaching biology at Southwestern (the answer is 18 years, since 2001), she very quickly shifted focus to talking about a “remarkable undergraduate” she taught years ago who is now an oncologist. When she publishes her research, she gives credit to every person who sends her samples because naming them as contributors will, she says, “help them get grants—and if they’re getting grants, that helps the whole community.” If you’re lucky enough to be one of her students or have a cup of tea with her, you’ll notice that she exhibits a generosity of spirit and that quintessential self-deprecatory Anglo-Irish sensibility that immediately draws you in.
And if you didn’t know any better, you’d almost never guess that this utterly unpretentious, quietly funny, and genuinely delightful individual is an expert in molecular biology and genetics who has made significant contributions to the progress of cancer research.

A “born biologist” whose first memory is of crawling down the garden path behind her London home and being “fascinated by ants and stones and leaves,” Todd recalls that her early love of science was the product of curiosity and exploration. “I remember as a child just staring at leaves and their veins, and my parents would allow me to dissect plants and flowers with kitchen knives,” she says. “I’d look at a beautiful flower, and then I would dissect it to see what was inside. I had to understand how it worked. I’m always appreciative of the beauty of nature, but I want to understand the mechanisms behind it.”
With the loving encouragement of her parents, Todd analyzed specimens she discovered in London parks and by the seaside, experimented with chemistry sets at home, and tinkered with gadgets her father would bring home from his work as an electronics engineer. She eventually enrolled as an undergraduate at the University of Sussex, where Todd originally hoped to specialize in conservation biology and ecology, following in the footsteps of her hero, Jane Goodall. But a first-year course on molecular and population genetics captured her imagination. “I knew then, at 19 years old, that this would revolutionize medicine, and I was completely seduced,” she recounts. “It changed my life.” So she traded romantic visions of a future examining ferns on the moors of England for a more fitting career at the lab bench studying genetic engineering.
Her studies would continue during a Ph.D. program at Cambridge University, where she lived for one year in the former home of the father of evolutionary thinking. “It was amazing to walk into the drawing room and think, ‘This is where Charles Darwin sat and read his newspapers and worked on the Origin of Species, and here am I, a little 20-something geneticist, sitting in the same window seat perhaps where he sat and looking out onto the grounds,’” she recalls. “It was a very magical experience.” She then adds with a laugh, “The rest of the accommodation was not magical and is best forgotten.” Todd admits that she did sometimes feel rather intimidated while at Cambridge, where she was one of only two women in her medical research cohort and worked in a lab flanked by a pair of Nobel Prize winners. Like so many graduate students, she was periodically afflicted with impostor syndrome, wondering whether her admission to the program had been some sort of mistake or even a cruel sociological experiment. But once she began to build a community among other women scientists at the university, her confidence grew, and she knew that she and her colleagues did, in fact, belong.
The importance of good questions
Todd shares stories like these with her Southwestern students, bringing profound empathy to her teaching and mentorship of students. “Most of my time is spent reassuring students, reminding them that they’re here for a reason, that they are good enough to be here, that they will excel here, that they are making a really valuable contribution to this community of learning, that we want them here, [and] that we’re learning from them just as they learn from us,” she says. “I always encourage students to ask questions and to share their ideas because their ideas might be the next great breakthrough.” It’s this approach to teaching that has understandably earned Todd multiple honors throughout her years at SU, including the Exemplary Teaching Award from the Board of Higher Education and Ministry of the United Methodist Church and the Southwestern University Teaching Award.

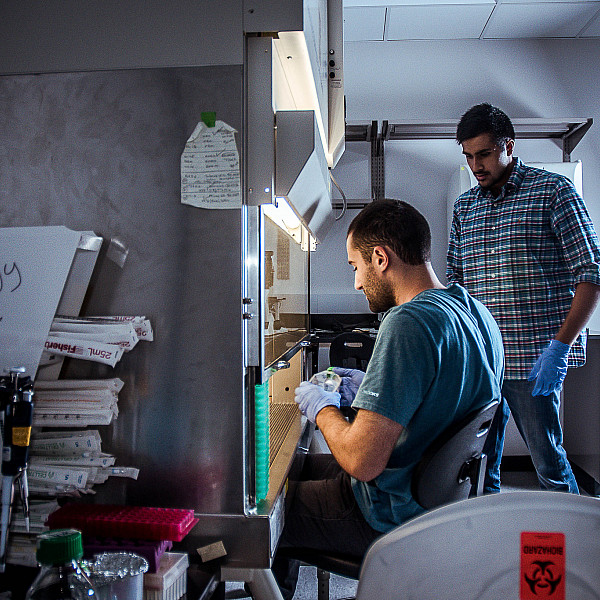
Biology major Anthony Seek ’20 agrees that the lab experience, even with all its “mental hurdles,” has been “pretty awesome” because it’s pushed him to consider not just the what but also the why of cell biology: “I wanted to do this before I came here, and I’m really excited I got the opportunity to do this and work with Dr. Todd. She’s amazing. I sat in on one of her classes before I came [to SU], and it was great. She’s the best person to work with.”
Todd’s appreciation for Solis and Seek is conspicuous as she praises them for being such independent thinkers and doers. She says that working with undergraduates is “fabulous” and “lovely” because “they bring youthful enthusiasm; they bring their curiosity. And something that I think is very special about undergraduates is that they ask questions that are quite basic, fundamental questions, and these are the best questions to ask in science.” She explains that as more advanced researchers delve deeper into their fields, they tend to think of more sophisticated, complicated questions. “But the best science is when we ask very straightforward questions, and students will do that, kind of pulling me up a little [because] maybe I had made an assumption about something … . They also ask questions about mechanisms and cellular processes that really keep me on my toes in terms of staying up to date with the literature.” And unlike how labs are often portrayed on television, Todd observes that “laboratories are communities; no scientist works in isolation. We’re highly collaborative, and we’re highly social creatures… . Our students bring life and heart to the lab.”
A common but understudied cancer
When students like Seek and Solis apply to work in Todd’s lab at Southwestern, they have to be highly conscientious, precise, and detail oriented. That’s because they’ll be working with complex instruments and techniques that are difficult to learn and require weeks to months of practice to master, or, conversely, they’ll be focusing for long periods on techniques that aren’t necessarily difficult but can be quite tedious.
Those students must possess physical and mental fortitude—not to mention a sense of respect for their materials—because they are working with cancer cells that are older than they are.
Todd and her students are studying uterine cancer, which, according to the nonprofit World Cancer Research Fund International, is the sixth most commonly occurring cancer in women (only breast, colorectal, lung, cervical, and thyroid cancers have higher incidences worldwide). More than 382,000 new cases of uterine cancer were reported in 2018, and approximately 76,000 patients die from the disease each year.
Although uterine cancer is the most common gynecological cancer in the U.S., it is, paradoxically, also the least studied compared with ovarian, cervical, vaginal, and vulvar malignancies—which is just one reason Todd and her longtime collaborator, fellow Southwestern Professor of Biology and Garey Chair in Biology Maria Cuevas, switched their research efforts from breast to uterine cancer several years ago while putting together an application for a National Institutes of Health grant. Todd believes “it’s one of those cancers that’s often overlooked by researchers” because “uterine cancer doesn’t have the same advocacy groups” that breast and ovarian cancers have enjoyed for the past 15 years. Those cancers have benefited from better research funding and more media coverage, likely because uterine cancer occurs less frequently than breast cancer does (one in 25 women versus one in seven, respectively) and is much easier to treat than ovarian cancer, which is often diagnosed too late to benefit from conventional therapies.
Todd says she and Cuevas were also compelled to refocus their research energies because they “found something very startling and very striking”: women of all races have about the same incidence of uterine cancer, but the mortality rate for African-American women with uterine cancer is 2-1/2 times that of all other women with the same disease. “We were completely blown away,” Todd recalls. “Why is it that the uterine cancer rate is not higher in African-American women but they die at much higher rates?”
Todd and Cuevas knew there were many possible answers: Perhaps African-American women were not being diagnosed early enough because of limited access to healthcare. Maybe cultural distrust between African-American women patients—of all socioeconomic classes—and their primarily white male doctors was preventing those women from advocating for their own care. And/or perhaps implicit bias was keeping patients from receiving sufficiently aggressive treatment. But these would be sociological responses and therefore beyond the scope of Todd and Cuevas’s research. From a biological standpoint, however, the pair could investigate which kinds of uterine cancer African-American women were being diagnosed with: Was it the more treatable endometrial cancer (i.e., malignancy of the lining of the uterus), or was it the more difficult-to-treat myometrial cancer (i.e., malignancy of the muscular wall of the uterus)? And if they were to look at tumor samples from women across racial identities, would they see differences in the ability of cancer cells to stay adhered to one another, or would those cells break off more frequently, making it easier for tumors to migrate through the bloodstream and spread (i.e., metastasize) to a different part of the body?
From cancer research to (better) cancer treatment
To help answer such questions about what causes cancer to spread throughout the body, Todd and her undergraduate research assistants—positions made possible by her funding as Southwestern’s first Ed and Suzanne Morrow Ellis Term Chair—work with immortalized uterine tumors from women. That is, normal cells eventually stop dividing, grow old, and die; cancer cells, however, have short-circuited that aging process, so they can grow and replicate in perpetuity. So when patients have a tumor removed, researchers can actually continue to grow and examine immortal cell lines derived from that tumor. Todd says, “I say that to the students: ‘Just think about what it is that you’re handling here in these flasks. These are cancer cells that are immortal, and they will outlive us and your children and your grandchildren.’ So we do treat them with a certain amount of reverence, actually.”
With all due reverence, Solis, Seek, and Todd are studying claudin-3 and claudin-4, just two members of a family of 24 tight-junction proteins that create watertight seals between adjacent cells and help hold those cells together. Although one might expect that having high levels of something called tight-junction proteins would mean that the connections between cells would be even stronger, it turns out that claudin-3 and -4 are abnormally elevated in uterine cancer cells, and that disproportion of proteins actually makes it easier for malignant cells to shear off, spread to another organ, and grow secondary tumors. Todd believes that down the road, if she and her fellow researchers can correlate high levels of claudin-3 and -4 with certain stages of uterine cancer, that correlation can prove useful not just as “a diagnostic marker” but also as a prognostic one. That is, a doctor could tell a patient how much cancer is in the body and better predict how the cancer will behave, including how it will respond to treatment.
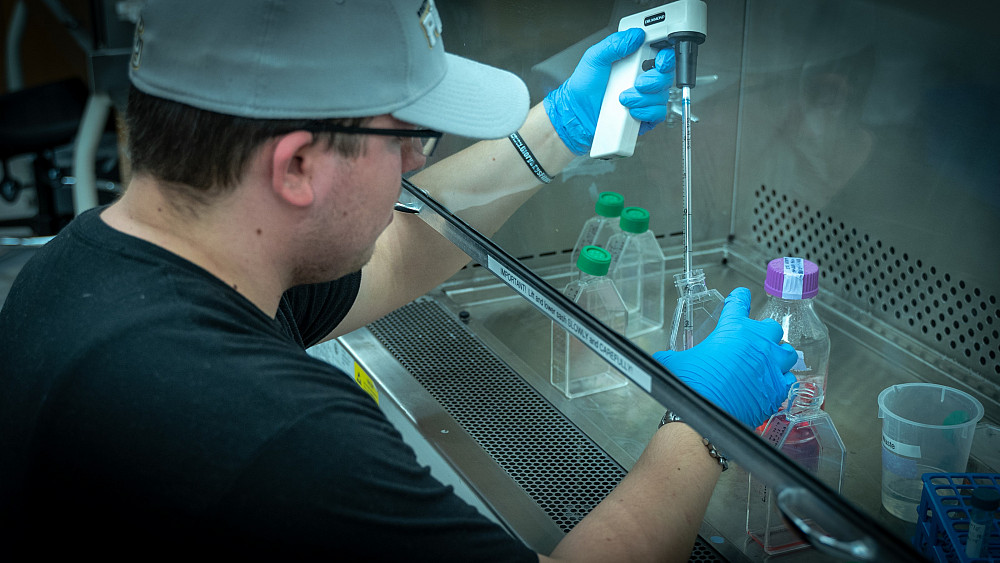
“But most exciting to me—and something that my lab and my students are working on—are the possible treatment applications,” Todd shares. She and her collaborators have been able to use a molecule known as small interference RNA to decrease the excessive amounts of claudin-3 and -4 to normal levels, which prevents the uterine cancer cells from migrating or moving across membranes as quickly. The hope, then, is that by decreasing the levels of these proteins, scientists will eventually be able to stop uterine tumors from metastasizing.
“That’s obviously my goal as a cancer researcher and I think the goal of most people who go into cancer research,” Todd says. “We might not see those clinical applications in our working lives, possibly not even in our lives, but we build on one another’s work.” She’s hopeful that gene therapies similar to those she and her students are experimenting with will one day complement conventional cancer treatments such as surgery, chemotherapy, and radiation. Or rather, given the physical and emotional trauma of surgery and the side effects and risks of chemotherapy and radiation—which can damage DNA, have adverse effects on neighboring healthy cells, and lead to mutations that cause secondary cancers—Todd adds, “I’m hopeful that in our children’s generation, gene therapy will be part of the treatment program, and by the time they have children, gene therapy will be the major tailored form of therapy and we will eliminate chemotherapy drugs or radiation altogether.”
In April 2020, Todd and Cuevas will present their research at the annual meeting of the American Association for Cancer Research, where the theme will be “Turning Science into Lifesaving Cure.” Todd looks forward to sharing their latest findings with their scholarly colleagues, and she’s thankful for her Ellis Term Chair funding because it will support her travel to the conference and because “it means that the research we can do at Southwestern is comparable to that at a large R1 [research] institution, and we’re really excited about that.” But she and Cuevas are also dedicated to translating their knowledge in ways that will benefit their students beyond academic or professional development. “In a biology class, it’s not just about preparing for medical school or graduate school or teaching or industry; it’s about learning about our own health, our own journey, and how our bodies change on a continuous basis,” Todd explains. “It’s just so important from an intellectual standpoint to understand the structures, the functions, and the mechanisms. But it’s also important from a very human perspective to understand the emotional component, the biological component, and the psychological component that contribute to our own well-being.”